|
The power of evidence: why proven therapies matter in pressure injury prevention
Tuesday, 18 November 2025
|
|
Pressure injuries continue to represent a major challenge across healthcare settings worldwide, impacting patient outcomes, length of hospital stay and healthcare costs. In pressure injury prevention (PIP), these experts say using evidence-based products and practices can dramatically improve outcomes for patients, healthcare professionals and healthcare organisations alike. This content is brought to you by our generous Platinum Partner Mölnlycke. 
According to Michelle Barakat-Johnson, Professor of Wound Care and Skin Integrity at the University of Sydney and Sydney Local Health District, the term evidence-based therapy refers to treatments and assessments backed by high-quality studies, such as randomised controlled trials (RCTs), systematic reviews and real-world clinical data. "When you rely on evidence, you're giving a patient a treatment or an approach that we know will work – not what we think might work," Professor Barakat-Johnson said. Sarah Sage, Clinical Nurse Consultant in Wound Management at the Royal Melbourne Hospital, agreed. "Medicine is meant to be the application of evidence to a clinical situation – and we're also meant not to do any harm," she said. "If we can't validate that a therapy works, we've got to make sure we're not hurting anyone." Ms Sage said the challenge for frontline staff is that they don't see long-term patient outcomes. "We might only have a patient for a day or two, so we need to know the products we're using are validated and effective," she said. Sonya Dick, Global Medical Affairs Manager for Prevention at Mölnlycke, said the shift towards evidence-based practice has reshaped modern wound care. "Evidence-based practice has long been accepted as the gold standard in most areas of medicine since the 1990s," Ms Dick said. "The prevention and management of pressure injuries now relies heavily on clinical guidelines and international standards; for example, the Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline ('The International Guideline') used the GRADE methodology to assess the quality of evidence supporting clinical practice1. "High-level, robust evidence has been transformative to patient outcomes – so it's critical for clinicians to adhere to these guidelines to deliver the best results for patients." From controlled trials to real-world resultsIn practice, healthcare professionals are encouraged to assess the hierarchy of evidence, often presented as a pyramid, with RCTs and systematic reviews at the top, followed by prospective and real-world clinical studies. "Controlled trials tell us if the intervention can work, but real-world studies tell us whether it does work," Professor Barakat-Johnson said. "And that's why we need both kinds of research." She said economic evaluations are equally important because they demonstrate whether a product is not only effective but also practical and cost-efficient. "Ultimately, the evidence should show that the product reduces pressure injuries, improves outcomes, and is realistic for everyday use," she said. 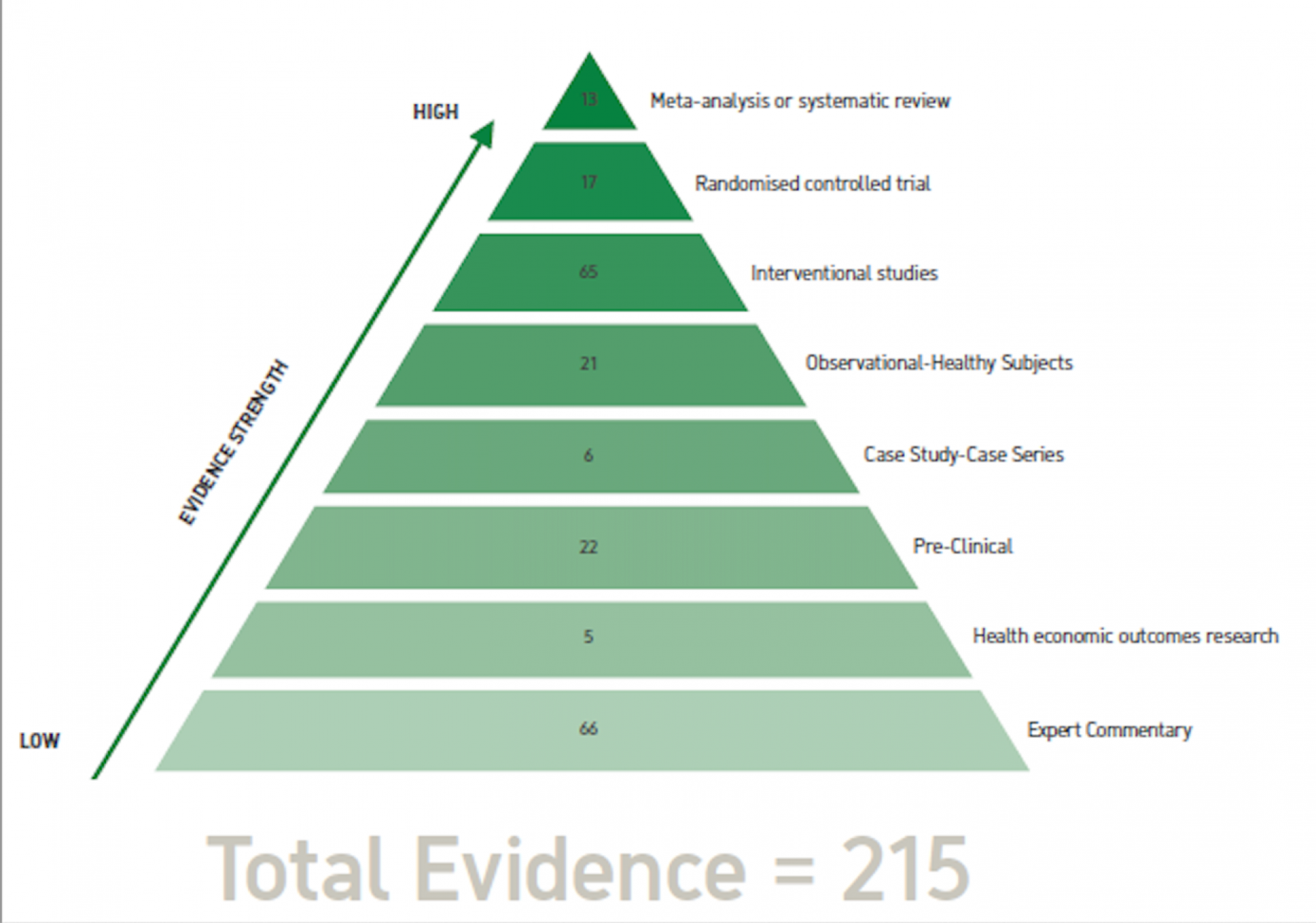
Pictured: The evidence hierarchy for Mölnlycke multi-layer Mepilex® Border foam dressings for pressure injury prevention. Note: Health economics outcomes research can sit anywhere on the evidence hierarchy, with trial-based evaluations usually higher, and observational or model-based studies usually in the mid-levels of evidence. Translating evidence into everyday practiceDespite strong evidence, implementation can be challenging. Ms Sage said not all prophylactic dressings or devices have the same quality of data behind them, meaning critical reasoning is vital. "We have to use clinical judgement – and sometimes we have to deviate from guidelines, but only for good reasons," she said. "It's not just about following the checklist; for example, I've seen a sacral dressing placed on a patient's lower back to avoid incontinence issues. "It might 'tick the box,' to say you're preventing a pressure injury but it's not doing the job it needs to do." Professor Barakat-Johnson added that systemic pressures – like staffing shortages and budget constraints – can hinder best practice. "Hospitals need to put measures in place that enable clinicians to deliver quality care through evidence-based practice," she said. "Policymakers should be listening to clinicians and considering solid evidence that links outcomes, patient dignity and cost savings." The economics of preventionFor policymakers and procurement teams, the message from experts is clear – cheaper isn't always better. "For every pressure injury prevented, money is saved and patient suffering is avoided," Professor Barakat-Johnson said. "We need to distinguish between price and value. A cheaper dressing that has to be changed more often will end up costing more and could potentially harm patients." Ms Dick said: "Value-based purchasing should consider not just the price per unit but the total cost of care. Studies using Mölnlycke products have shown that even with higher upfront costs, the overall cost to the healthcare system is significantly reduced." When research drives real changeProfessor Barakat-Johnson's Hospital-Acquired Pressure Injury (HAPI) research demonstrates that evidence-based programs can translate to significant impacts. The research team implemented a comprehensive PIP intervention across Sydney Local Health District, replacing plastic sheets and underpads with correctly fitting incontinence products, standardising supplies, using prophylactic Mepilex® Border dressings for high-risk patients, and introducing therapeutic beds, education and district-wide collaboration2. The results were striking. In 2019, the initiative led to a 51.4% reduction in incidence, a 71.6% reduction in prevalence, and a 23.1% cost reduction, saving more than $837,0002. Five years later, the incidence of hospital-acquired pressure injuries had dropped by 32.6%, and severe (Stage III–IV) cases by 27.3%3. "If we applied the numbers we found to other cost-efficiencies including hospital re-admissions due to pressure injuries, we estimate a saving of $4.5 million a year for our district," Professor Barakat-Johnson said. The value of evidence-based careFor healthcare professionals like Ms Sage, the benefits of evidence-based care go beyond numbers. "For patients, it means fewer and less severe pressure injuries, faster recovery and shorter hospital stays," she said. "For staff, it means confidence that we're doing the right thing – and less guilt when things go wrong. "For healthcare organisations, it's about reduced costs, better resource allocation and improved discharge planning." Still, misconceptions persist, particularly the belief that all prophylactic dressings are the same. "Not all dressings are the same," Ms Sage said. "The International Guidelines recommend using a multi-layer silicone foam dressing for PIP14, but there are differences in the different brands and it's very hard to find the evidence that they perform in a similar way. "So it's up to healthcare professionals to explain to the business decision-makers that not every foam dressing is the same and they don't all have the same levels of evidence behind them." Ms Dick said: "Prophylactic dressings can differ greatly in construction and technology. For example, Mölnlycke Deep Defence™ technology, which is proprietary to Mepilex Border Sacrum and Heel dressings, provides optimal strength and flexibility to protect against shear and friction5." Ms Sage illustrates the importance of tailoring evidence-based care with a personal example. "I had a patient who was a below-the-knee amputee with a Stage 1 pressure injury," she said. We trialled several dressings, and the one he found most comfortable – and that didn't interfere with his prosthetic – was the Mepilex Border Flex Lite. "The key is to evaluate evidence critically, apply it appropriately and tailor interventions to each patient." Proving what worksThe power of evidence-based products was demonstrated in the landmark Border trial, in which Ms Sage participated. The randomised controlled study compared standard care with the use of Mepilex Border Sacrum, Mepilex Heel and Mepilex Border Heel dressings in critically ill patients6. "We found that patients who received prophylactic dressings had significantly fewer and less severe pressure injuries, and those that did develop took longer to appear6," Ms Sage said. "It provided strong, validated evidence for their effectiveness." As these experts make clear, the future of PIP lies in combining science, clinical judgement and compassionate care. When products are backed by rigorous research – and health professionals are empowered to use them appropriately – the result is a win for healthcare systems and staff, as well as patients. Find more information and expert advice in the Mölnlycke Pressure Injury Centre. This content is brought to you by Wounds Australia Platinum Partner Mölnlycke (AUWC_002122) and is intended for healthcare professionals. References: 1. National Pressure Injury Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries. The International Guideline: Fourth Edition. Emily Haesler (Ed.). 2025. Available from: https://internationalguideline.com. 2. Barakat-Johnson M, Lai M, Wand T, White K, De Abreu Lourenco R. Costs and consequences of an intervention-based program to reduce hospital-acquired pressure injuries in one health district in Australia. Aust Health Rev 2019;43(5):516-525. doi: 10.1071/AH18131. 3. Barakat-Johnson M, Lai M, Graham J, Hallahan A, Coyer F. The "HAPI" project five years on: incidence and prevalence of hospital-acquired pressure injuries in one local health district in Australia. J Tissue Viability 2025;34(1):100846. doi: 10.1016/j.jtv.2024.12.010. 4. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA: 2019. 5. Alten. Finite element analysis studying the effect of different prevention dressings on protecting soft tissues from high stresses and deformation. Ref No. 001. Data on file. 2017. 6. Santamaria N, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T, De Vincentis S, Ng AW, Manias E, Liu W, Knott J. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. Int Wound J 2015; 12:302–308.
|
